The Hidden Struggle
A delve into coeliac disease

A daily struggle
‘Sorry, we can’t cater for you right now.’
That sentence cut a little deeper today.
Imagine. It was one of the hottest days of the year but, for you, it was also the first day volunteering at Glastonbury Festival. And of course you’d been working in direct sunlight all day.
‘Can I see your ticket?’ Seems to be the only sentence you have uttered all day.
Finally, freedom for the evening is offered. Who’s performing later? George Ezra? Stormzy?
But right now, food is the main thing on your mind. You literally haven’t sat down all day.
Your heart drums inside your chest as the food stalls enter your field of vision. Are you about to pass out from hunger or is it just the bass of distant music you can hear? Is that Bastille?
Food.
Food.
Food.
Noodles, burgers, pizza, paella. French, Italian, Chinese, Thai. The smells, the flavours, the choice. Which stall do you pick?
To be honest, it doesn’t matter.
'We’ve sold out of the gluten free option.'
Stall after stall, step after step, hope fading and frustration growing after each vendor gives you a regretful ‘No.’
'We didn’t think the gluten free option would be so popular.’
But it’s not a case of popularity for you, it’s a necessity.
‘We have a vegan option if that works?'
But no, of course that doesn't work.
Waves of people pass you by, clasping their biodegradable containers that enclose some delicious goodie within. You bet they didn’t have any trouble finding food. The smell lingers.
Your mouth waters in the spirit of 'if only.'
But there is no 'if' for you. The consequences are not worth it.
Maybe there will be more tomorrow.
You don’t eat today.
My sister didn’t eat that day.

Anna working at Glastonbury (2019).
Anna working at Glastonbury (2019).

Designed on Canva
Designed on Canva
It is estimated that 1 in every 100 people in the UK have coeliac disease. And when you realise there are roughly 68.86 million people in the UK, that is a lot of people!
When my sister Anna (now 23) was diagnosed back in 2018, I'll be honest and admit that I had no idea what it was.
‘So you can’t eat bread?’
I think that was the extent of my understanding.
So, what is coeliac disease?
Coeliac disease is an autoimmune condition. It is when the body's immune system attacks its own healthy tissue if gluten is eaten. If someone with coeliac disease eats gluten, their immune system damages the lining of the small intestine.
Symptoms can range from mild to more severe.
Common symptoms include: diarrhoea, constipation, stomach ache and tiredness.
Other symptoms include fatigue, weight loss and ataxia (a lack of co-ordination).
The diagnosis process involves getting a blood test to check for certain antibodies.
The next step is an endoscopy/biopsy. Gastroenterologists take a small sample of the small intestine lining to examine under a microscope.
Afterwards, it will then be confirmed if the patient has coeliac disease.
*New guidelines, published due to Covid-19, mean that in some cases people can be diagnosed without the need for a biopsy.
*Gluten must be eaten during the process of diagnosis.
There is no cure for coeliac disease.
Coeliac disease is treated by following a strict gluten free diet.
If someone with coeliac disease continued to eat gluten, this could lead to:
Malnutrition: This is when a lack of nutrients are absorbed, due to the digestive system performing less efficiently. This can lead to dizziness, confusion, fatigue and, for children, delayed development and stunted growth.
Malabsorption: This is when vitamins and minerals are not fully absorbed. This can lead to anaemia and osteoporosis (when bones become brittle and are weakened).
If a person with coeliac disease was misdiagnosed or continued to eat gluten, there can be many long-term implications:
Lactose intolerance: There is an increased risk of developing lactose intolerance if a gluten free diet is not followed.
Infertility: There is an increased risk of struggling to conceive, the chance of miscarriage and pregnancy complications.
Cancer: There is a rare, but increased risk of developing small bowel cancer, small bowel lymphoma and Hodgkin lymphoma.
Despite not having coeliac disease myself, the impact of my sister having the condition was huge. Things I’d never given much thought to became banned in our house.
‘Did you just use that knife on your toast and put it back in the butter?’ Not allowed. Cross contamination.
‘Did you just put my pizza on the same tray as yours?’ Not allowed. Cross contamination.
‘Did you just dip your crisps into this salsa?’ Not allowed. Cross contamination.
Maybe it doesn’t seem like a huge impact, but habits are hard to break. And having to teach myself new ones, after years of the same routine, was something that I found challenging.
And I have no doubt that it was far worse for Anna.
At the age of eighteen, all of the foods that she once loved and grew up eating became the very thing that was making her ill.
And the difference between me and her is that, when we are apart, I can forget all of those food related worries. But she will never be able to leave those concerns behind.
The Hidden Struggle: A delve into coeliac disease. This is part one of a three-part mini-series about coeliac disease. In this podcast, I am joined by: Cristian Costas Battle – Gastroenterology dietitian who specialises in coeliac disease. And Annabel Wellington – Personal trainer and online coach, diagnosed with coeliac disease in her childhood. In this episode, we will be discussing the diagnosis process and life after being recently diagnosed.
Designed on Canva
Designed on Canva
As we just heard from Cristian, the average time it takes to be diagnosed with coeliac disease is thirteen years. And even though that is not always the case, getting a diagnosis can be a difficult and confusing process.
He also explained that ‘up to 25% of people living with coeliac disease have previously been diagnosed with IBS (irritable bowel syndrome), simply because the digestive symptoms are so similar.’ With these ambiguous symptoms and the high possibility of a misdiagnosis, there is no surprise that some people face major struggles when it comes to getting their correct diagnosis.
Coeliac disease - diagnosis stories

Niki Pappas - 28
Niki Pappas - 28
'My negative experience actually revolves around getting diagnosed. When I was 18, I lived in the USA and I would have really bad abdominal pain, but that was always blamed on PMS. But then one day, it got so bad that I went to the doctors and was eventually told that I had coeliac disease. The doctors didn't really stress the importance of the condition, so I did not feel like I was very informed. I was then later retested for coeliac disease and this time, they told me it was negative! However, after moving to the UK, I experienced really bad dermatitis all over my body and was always bloated. I was then diagnosed with osteopenia. Just after my 26th birthday, a GP here re-diagnosed me with coeliac disease. It has been a long and frustrating journey.'

Archie Hollyfield - 34
Archie Hollyfield - 34
'In 2019, I was actually diagnosed with ulcerative colitis and two years later I had a really bad flare up. My doctor referred me to a gastroenterologist and, in March last year, I had a consultation and a letter saying that I was scheduled for an endoscopy. I showed up on the day and they said it was to test for coeliac disease - no-one had mentioned this to me before! I then didn't hear anything until September 2022, when I received a letter saying I had coeliac disease. I got a booklet and a video to watch about the condition. I do feel like I've been left to my own devices a lot, but I'm sure the support would be there if I did reach out.'

Callum McGuiness - 21
Callum McGuiness - 21
'I was only diagnosed in March 2023. I had suffered a lot with constant fatigue but, after going to the doctor, I was actually diagnosed fairly quickly. It took around eight months from my first blood test, to when I was officially diagnosed. I don't know if you could call it a bad experience, but I was literally just sent an online message to say that I had coeliac disease. And that was it. I have now been referred to a dietitian, but I haven't been given an appointment yet. I have found it quite daunting and feel very anxious going out, as I don't really know what I should be looking for.'
Warning: this section contains sensitive content surrounding eating disorders.
Any new diagnosis, especially one that revolves around food, can have some major knock-on effects to personal confidence.
At only 25 years old, Laura Harry is still dealing with the unanticipated effects of her coeliac disease diagnosis she received at 17.
‘For those first few weeks after getting diagnosed, I was petrified of food. I wouldn’t go near it.’
Laura struggled with restrictive eating after getting diagnosed in 2014, and later developed an eating disorder. She recalls not being told much about cross contamination, so experienced getting ‘glutened’ regularly, which instigated her fear of food.
*’Glutened’ is a term that is used when someone with coeliac disease accidentally consumes something containing gluten.
Currently living in Swansea, Laura is soon to begin her master’s degree in psychology, where she hopes to research the link between coeliac disease and eating disorders.
‘I was never offered any professional help.’ Laura speaks matter-of-factly, as if she is telling a story of someone else’s life, but her eyes are the giveaway – full of disappointment, as she recalls the obstacles her younger self had to overcome alone. She pauses with deep thought and reflection, as she carefully considers her words.
‘In a way, I’m glad for my eating problems, otherwise I probably wouldn’t have seen a dietitian.’
After Laura’s diagnosis, she began her gluten free diet. ‘I started putting on weight as I was healing from the internal damage that gluten had been causing me. But at the same time, my fear had made the connection that food made me ill, so I just spiralled in my eating disorder.’
Despite this, Laura did take the leap to access support for her eating disorder. Although, this led to her feeling even more isolated and misunderstood. ‘They [eating disorder clinic] just told me to stop using the fact that I can’t find safe foods as an excuse not to eat.’
Online, the main source of support for those that suffer with the condition is Coeliac UK. Established in 1968, this charity assists those with coeliac disease and other gluten intolerances, with the goal that ‘one day, no one’s life will be limited by gluten.’ Here, people can be signposted towards resources, information and even a helpline. However, they do highlight that after being diagnosed with coeliac disease, GP’s should refer patients to dietitians to help support their transition into a gluten free lifestyle.
Luckily, Laura was able to work through her eating disorder. But, as a result of her experience, she decided to set up an Instagram account to connect with others and build a support network. She is amazed at how many people have had similar experiences with restrictive eating.
If you have been affected by any of the issues raised, please visit Beat UK for additional help and support.

Credit: Laura Harry
Credit: Laura Harry

Source: interview with Laura Harry
Source: interview with Laura Harry
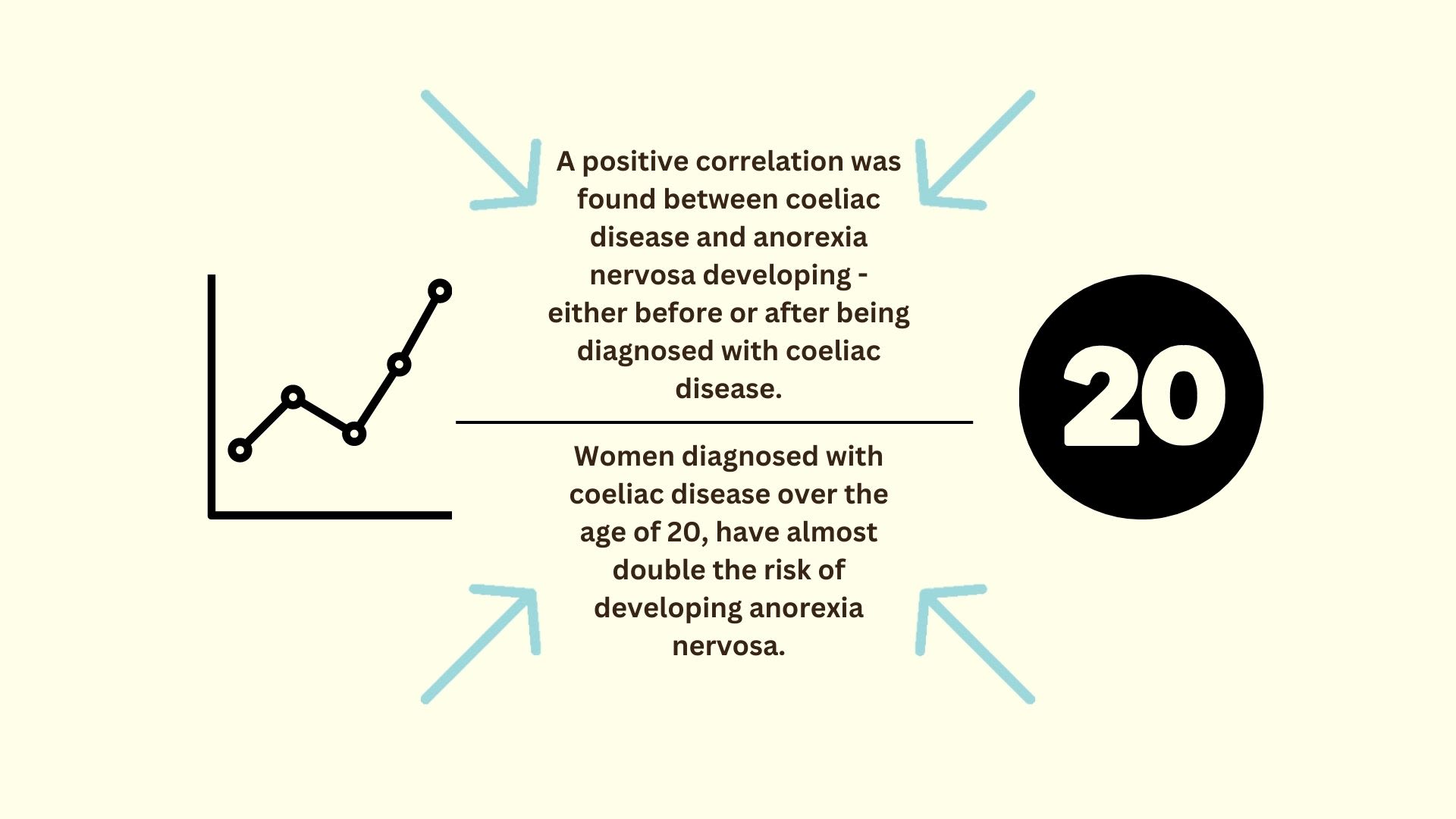
In 2021, Riccardo Dalle Grave, Head of the Department of Eating and Weight Disorders at the Villa Garda Hospital, wrote the article ‘The Coexistence of Eating Disorders and Celiac Disease’. He detailed how coeliac disease could trigger the development of an eating disorder and how, living with both coeliac disease and an eating disorder ‘increases the likelihood of developing severe complications of coeliac disease’.
He also referenced a study that was conducted using the Swedish National Patient Registry. In 2017, a group of researchers used this registry to study the link between coeliac disease and anorexia nervosa and found a strong correlation. They concluded that this link should be heavily considered during the diagnosis process and any follow-up appointments. Unfortunately, there is still a lack of professional research in examining this correlation in-depth.
Despite Laura and Anna being diagnosed in their late teens, coeliac disease can develop at any point in a person’s life – including childhood.
In 2022, Coeliac UK announced their ‘No More Lost Childhoods’ campaign – aiming to help parents identify signs of the disease. They found that 25% of children in the UK had to wait over two years to receive a diagnosis. But for children that are silently struggling, eating gluten can lead to stunted growth and delayed development. Heidi Urwin, Director of Evidence and Policy at Coeliac UK, said that this diagnosis delay in children was partly due to ‘a general lack of awareness of the key symptoms of coeliac disease.’
And unexpectedly for Debbie Bath, it was only after her three year old son was admitted to hospital with pneumonia, that they found out he also suffered with coeliac disease.
‘He was admitted in October last year and he was also anaemic, so they did lots of blood tests. But it wasn’t until March that he was officially diagnosed.’
Her son has now been referred to a gastro-paediatrician and dietitian, but they are yet to hear anything back.
‘The only advice we’ve been given, is to follow a gluten free diet and look at Coeliac UK for more information. But for a little boy who’s been very poorly due to anaemia and a damaged gut lining, I just don’t think that’s good enough.’
Despite this, coeliac disease is actually more frequently diagnosed in people between the ages of 40-60 years old. But this presents even more struggles and challenges, as people try to adapt to their new condition.
Designed on Canva
Designed on Canva
Source: beyondceliac.org
‘I thought my life was over.’
Linda Brown, 58, lives in Australia and was diagnosed with coeliac disease fifteen years ago. However, she suffered with tiredness and stomach aches since her early twenties.
‘My GP could never find the cause of my symptoms and then, after having my baby at 32, I was told it could be post-partum depression.’

Credit: Linda Brown
Credit: Linda Brown
‘It was only at 43 that I needed a blood test for an unrelated issue, they told me I had coeliac disease. I remember bursting into tears, but now I realise it was the best thing that could’ve happened to me – I feel better at 58 than I ever did at 40!’
Now, Linda has higher energy levels and no pain when she eats, but she admits that the diet was hard at first – especially when eating out.
‘I used to be quite shy about it, but I’ve had to learn to speak up for myself and double-check everything. It can get quite tiresome, but I need to do it to ensure I won’t be glutened.’
And having access to these safe foods is probably one of biggest struggles that those living with coeliac disease have to face.
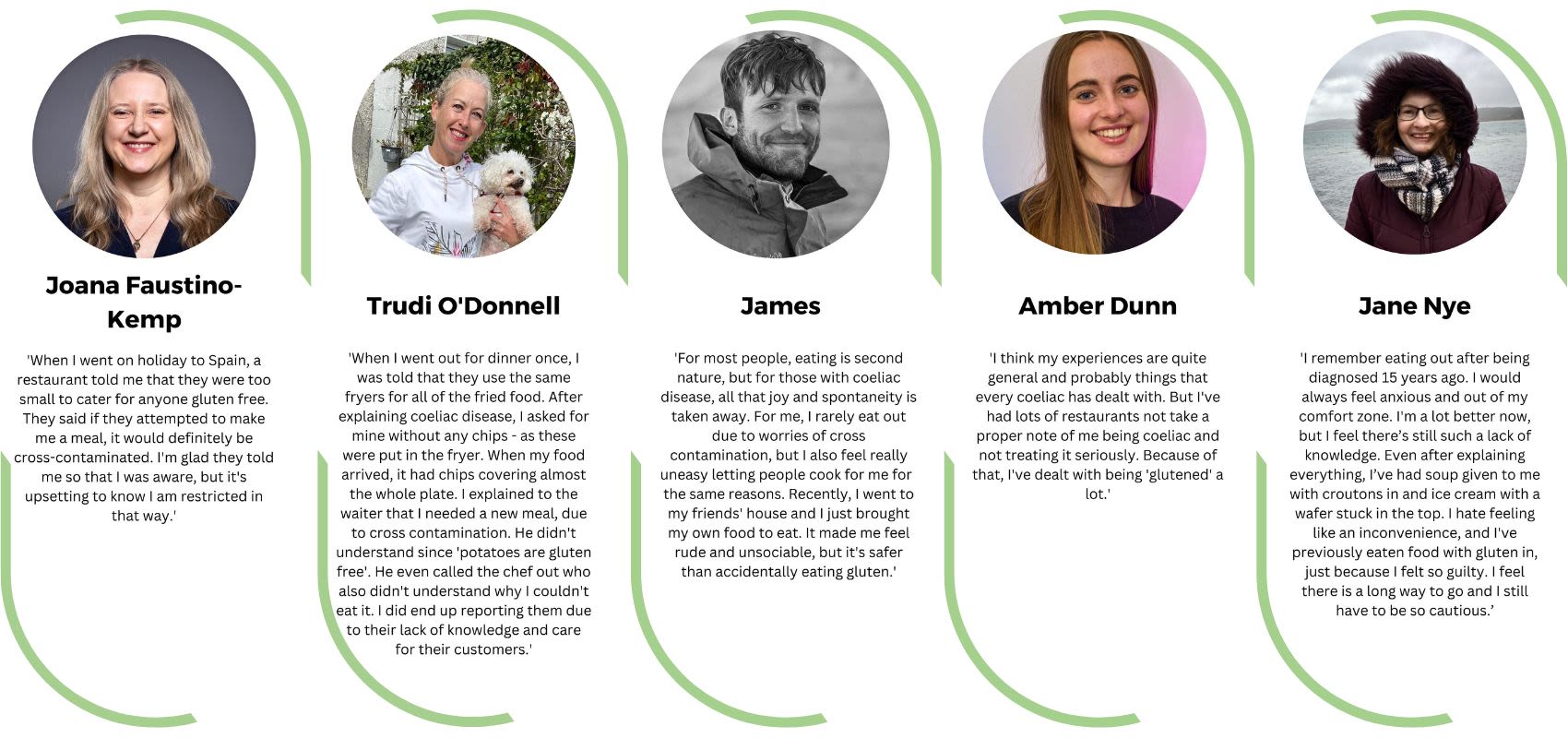
The eating out struggle
Eating out can be something that a person does for many reasons. Or maybe for no reason at all.
Celebrating birthdays, a wedding, a ‘work do’ or a spontaneous trip out – chances are, that food is going to be involved.
For most people, not a second thought goes into it.
But when you are coeliac this isn’t the case and, more often than not, you are researching to see if you can even be catered for.
Spontaneity just isn’t an option.
Also, while some venues offer gluten free options, the presence of gluten in other dishes means there is a possibility of cross contamination. So, with the risk of not finding anything to eat or even being glutened by what is eaten, it is no surprise that there can be a lot of anxiety around eating out.
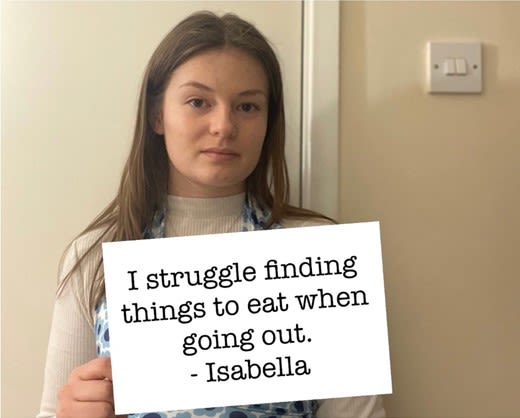
Credit: Isabella Alderson
Credit: Isabella Alderson

Credit: Andrew Marchment
Credit: Andrew Marchment
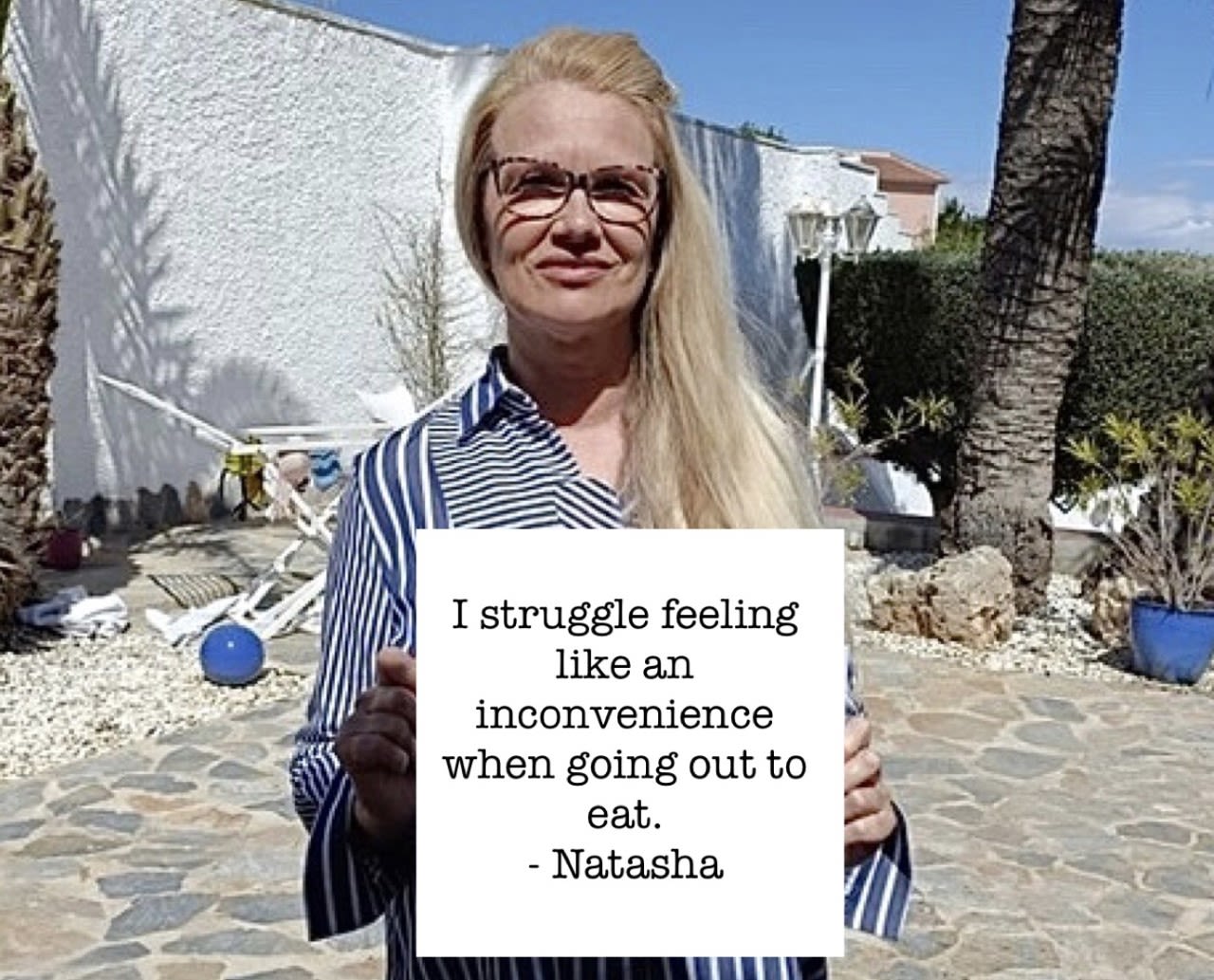
Credit: Natasha Grocutt
Credit: Natasha Grocutt
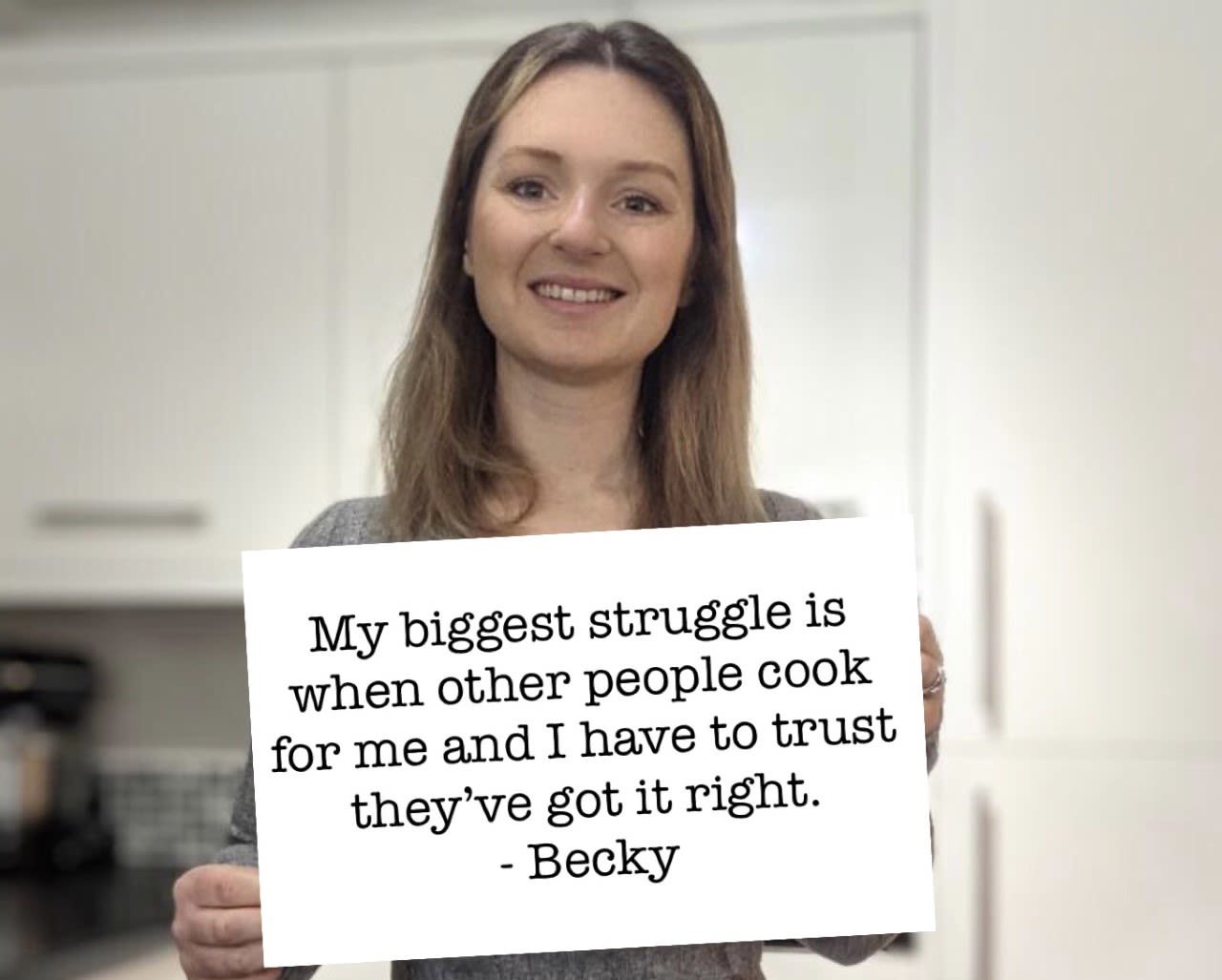
Credit: Becky Kiddle
Credit: Becky Kiddle

Credit: Kath Walters
Credit: Kath Walters
Geraint Evans lives in Abergavenny and was diagnosed with coeliac disease when he was a young child. He does not remember a point in his life where he could eat gluten, but he believes this makes living with coeliac disease a lot easier.

Credit: Geraint Evans
Credit: Geraint Evans
‘When people are diagnosed later in life, they miss all the foods they can’t eat anymore. For me, I don’t really know any different.’ As he speaks, he offers a small shrug of acceptance.
Despite this silver lining, Geraint finds that he mainly struggles abroad.
‘I love to travel, but not being able to eat gluten makes everything ten times more difficult.’
Geraint and his wife recently travelled to New York but, before they went, Geraint completed meticulous research to find out where he could eat – for every single day.

Geraint in New York
Geraint in New York
‘Even though I’m the one who can’t eat gluten it impacts everyone around me, especially my wife as we can never just go out spontaneously.’
However, Geraint acknowledges that this added workload of research, just to safely eat, ‘it’s all part of being coeliac’.
But, growing up gluten free and being diagnosed later on in life, must be a very different experience.
Laura Harry, who suffered with an eating disorder after being diagnosed with coeliac disease later on in life, believes that the freedom to go out is the biggest impact her diagnosis has had.
‘When I was first diagnosed, I hated feeling like an inconvenience and making people cater for me wherever I went. There were times that if my friends booked a restaurant that couldn’t cater for me, I’d just risk it even though it could make me sick. And then that played into the whole fear of foods, but my priority at the time was not to miss out.’
These days, Laura sticks closely to her gluten free diet, but admits that she still struggles to go out to eat.
‘There are so many times that I’ve pretended to be ill or busy, because it gets to a point that it’s easier to let my friends go out and just stay home and cook for myself.’
Laura believes that those who do not have coeliac disease, do not understand – or even consider – the massive effect it can have on people’s lives.
‘Being coeliac impacts your mental wellbeing, your social life and just everything.’
Designed on Canva
Designed on Canva
With 1 in 100 people living with coeliac disease in the UK, most of these people want to know that when they go out to eat, their dietary needs will be taken care of.
And The Red Lion pub in Badlesmere does just that.
Owner and chef Paul Burton, moved his pub’s location back in 2017. He heard from the previous owners, that a lot of customers were gluten intolerant and would choose the gluten free options they provided. Paul decided to use this new move to take that idea one step further. Instead of offering a selection of gluten free options, he decided that the pub would be 100% gluten free.
‘Initially it was kind of an experiment to see if people would even notice. And it’s not like it really affected us, it’s all the same pub classics, just without gluten.’
What started as an experiment is now a pub in its sixth year, serving only coeliac friendly food.
The Red Lion has been approved by Coeliac UK, which means that they are trusted to serve gluten free meals, without the risk of any cross contamination.
Paul said that for the first three years of the pub’s opening, they were the only independent pub on the Coeliac UK website. As a result of that, the pub has seen customers who have travelled from across the UK, just to be able to eat at a fully gluten free establishment.
‘We have people who get really emotional, simply because they feel fully safe to eat, which they may have not experienced before. Not only can they share and taste someone else’s’ food, but they don’t even have to think about cross contamination. It’s something that most people take for granted.’
The one downside of serving an entirely gluten free menu, is the slight price increase.
‘To be honest a standard menu is probably already 80% gluten free, but it’s that 20% that is more expensive. I mean, I have to order my bread from Scotland and have it delivered down here.’
Despite the slightly more expensive ingredients, Paul does not charge his customers more as he believes everyone should have access to the same standard of food and price point.
‘At the end of the day, people can’t help being coeliac and I’m not going to charge them more just because they happen to have the condition.’



The eating in struggle
Cooking at home can ease many worries about eating out, such as the chef messing up a gluten free order or not even finding somewhere to eat.
But it can also come with a completely new set of obstacles. Getting ingredients off the shelves and into the kitchen may not be as easy as you think.
Many supermarkets have ‘Free From’ sections, where a range of food that doesn’t contain gluten can be found. However, not all gluten free foods are kept there, and some options may be hidden amongst the shelves.
Checking ingredients and looking for the dreaded ‘may contain gluten’ label, to figure out what foods are safe to eat, can be a time-consuming task.
This struggle is something that has been recognised by Coeliac UK, who offer the Live Well Gluten Free app and website. Here, people can search different products to see what foods are safe to eat.
Heather McCaw, Food Information Officer at Coeliac UK, works with manufacturers and the public to ensure that their information on products is up-to-date and accurate.
As a coeliac herself, Heather understands the stress that can occur when people are unsure what is safe to eat, so aims to ensure that people can trust Coeliac UK’s guidance and ‘do not let their dietary restrictions hold them back.’
As well as making sure the database information is correct, Heather also deals directly with members of the public, who call to ask about specific products.
‘Unfortunately, people do ring up simply because they get so overwhelmed with figuring out what they can eat. People can be so frightened of ingesting gluten that they just need that added clarity and, at Coeliac UK, it is our job to help them.’
As Heather helps people figure out what products are safe, there are other obstacles that may be holding people back.
In general, gluten free alternatives already cost a notable amount more and, with the cost-of-living crisis, this is only getting worse.
Gluten free vs gluten containing
Prices found in April 2023.





Designed on Canva
Designed on Canva
A spokesperson for Warburtons (baking company) stated that, while they work hard to sell products at the best possible prices, ‘our gluten free products are more expensive to produce, mainly because the process is very labour intensive.’
Additionally, Schär – the long-standing international brand known for creating gluten free products – has suffered the effects of the cost-of-living crisis. A spokesperson said, ‘we’ve recently experienced significant cost pressures and in order to be able to continue offering our consumers the highest quality products, we have taken the difficult decision to increase our product prices. We will continue to do everything we can to mitigate costs.’
In March 2023, Coeliac UK released the report ‘The gluten free diet – How much does it cost and why does it matter?’ Within this, the high cost of gluten free products, and concerns that people may not be able to afford the food they rely on, are highlighted.
The report is part of Coeliac UK’s #GFCostPledge campaign, to help make gluten free food more affordable because, as Dr Jeremy Woodward (Consultant Gastroenterologist) said: ‘The added expense of having a diagnosis of coeliac disease may become unsupportable.’
The Hidden Struggle: A delve into coeliac disease. This is part two of a three-part mini-series about coeliac disease. In this podcast, I am joined by: Cristian Costas Battle – Gastroenterology dietitian who specialises in coeliac disease. And Annabel Wellington – Personal trainer and online coach, diagnosed with coeliac disease in her childhood. In this episode, we will be discussing the cost-of-living crisis while living with coeliac disease.
As Cristian explained, in parts of the UK (excluding England), those diagnosed with coeliac disease can access gluten free products on prescription, such as bread, flour and pasta. However, the availability of prescriptions in England varies greatly. Only bread and flour mixes may be offered and, in some areas, these prescriptions are not provided at all.
Tristan Humphreys, Head of Advocacy at Coeliac UK, works with policy makers to help promote positive change in the coeliac community. He recognises that prescriptions in England are a complete ‘postcode lottery’ and are a barrier for many people trying to adhere to their gluten free diet.
Tristan explains that advocating for prescriptions is a long, ongoing and complicated process, as the availability of prescriptions is decided upon by each Clinical Commissioning Group (CCG) in England.
Despite these current obstacles, Tristan explained how Coeliac UK is currently calling on policy makers to help and support those with coeliac disease overcome these barriers.
And additional support from the government, may be exactly what is needed.
Source: interview with Tristan Humphreys
Source: interview with Tristan Humphreys
The struggle from above
Where there is a struggle, there is also a fight.
That even applies to coeliac disease.
For many years, Coeliac UK has recognised the difficulties that come hand in hand with the condition. And, as both a charity and patient representative, they continue to find ways to offer support and ease daily struggles. They provide free information on a range of topics, such as how to cope with diagnosis, local support groups and offering travel guides. But it is not just information they provide. Coeliac UK doesn’t just want to help people navigate ways around a glutenous society – it is real institutional change that they are after, and advocating for this goal is something Tristan Humphreys knows too well.
As Head of Advocacy at Coeliac UK, Tristan works within the Evidence Policy team, but there are many different sectors within this team too – these include food policy, health policy and research. All of which have very different purposes, for example securing funding, engaging with healthcare professionals and providing food safety schemes. Despite this, the same overarching goal is shared – to create positive changes for those with coeliac disease.
But in his position, Tristan’s role goes above and beyond simply asking policy makers for change.
'Advocacy is all about taking the knowledge within our team and using it to influence those people in power. But often, you’re building those relationships so that, when the time comes, you have a foot in the door and can apply pressure when needed.’
Tristan Humphreys
The most recent work that Tristan has been involved with is Coeliac UK’s cost campaign. Not only has he approached individual commissioners and the Department of Health to discuss prescriptions in England, he has also been in discussions with retailers to help them commit to affordable access to gluten free products.
Unfortunately, as a lot of Tristan’s work is to do with policy, results do not occur overnight. Instead, there is a lot of long-term negotiation, planning and discussion involved.
In addition to this work, Tristan also supported the re-establishment of the All Party Parliamentary Group (APPG) on coeliac disease in November 2022 – after the group was previously disbanded due to a loss of members. APPG’s are cross-party, special interest groups who work in Parliament to help drive policy changes and, in this particular one, issues related to coeliac disease are discussed. Later in 2023, the APPG have plans to launch an inquiry into diagnosis process of coeliac disease and present a report to Parliament.
However, within all of his work, Tristan believes that the hardest aspect is that people simply do not understand the severity of the condition.
‘A gluten free diet is a medical necessity, not a lifestyle choice. And the bottom line is that it’s totally doable for every caterer and venue to provide gluten free food safely, but it’s a lack of knowledge and commitment that’s holding them back.’
He also said that ‘we are still seeing a challenge in terms of hospitals and schools too. It is important that the condition is treated with the severity that it merits and that there is recognition that people with coeliac disease require support.’

The Hidden Struggle: A delve into coeliac disease. This is the final episode of the three-part mini-series about coeliac disease. In this podcast, I am joined by: Cristian Costas Battle – Gastroenterology dietitian who specialises in coeliac disease. And Annabel Wellington – Personal trainer and online coach, diagnosed with coeliac disease in her childhood. In this episode, we will be discussing support and the future for those with coeliac disease.
As Annabel just said, while growing up she experienced being isolated from her friends during school lunches, simply because she had coeliac disease. This understandably led to her feeling very singled out and encouraged her to develop negative connotations with eating.
Luckily today, there are more provisions in place to support children with medical conditions (such as coeliac disease) at school. Not only that, but it is also the law. Section 100 of the Children and Families Act 2014, states that schools have a ‘statutory duty’ to make arrangements for such children and should have a policy in place for managing long-term health conditions.
The versatility of Coeliac UK is demonstrated in this instance too, as they also help educate schools on the condition and can provide specific resources. As Cristian highlighted, ‘charities like Coeliac UK are completely key.’ The work that they do, such as their fundraising and research, is especially important.
As a charity, their work relies on funding and donations, and they have been able to make their name as the largest funder of coeliac disease research in the UK.
Tristan Humphreys explained how significant research has already been supported by Coeliac UK over the years, and they have plenty of research currently ongoing and upcoming. He is most excited by the research by Dr Elizabeth Soilleux, to find a faster and better solution to the diagnosis process of coeliac disease. Her team is developing an artificial intelligence solution to diagnose the condition, which they hope will help fast-track diagnosis and potentially help identify other conditions.
In addition to this, there are many different areas of research that Coeliac UK funds – from diagnosis, the impact on the immune system and even the quality of gluten free bread. But Tristan says, it is the efforts to find a cure that the community is most interested in – and the CEO too! Chief Executive, Hilary Croft, has recently said that it is her ‘personal mission’ to ensure that a cure for coeliac disease is found.
This hope is most certainly shared amongst most of the coeliac community.
As for other aspects of the future, Tristan hopes that there will be clearer guidance for people to follow – from diagnosis to the ongoing management of the condition. He also hopes that gluten free products will become more readily available and affordable to those who need them, to ultimately ensure that one main aim is met.
That nobody is left struggling alone.







Designed on Canva
Designed on Canva